Why Early TBI Rehabilitation Matters After a Car Accident in Kansas City
Traumatic brain injuries are some of the most misunderstood and underdiagnosed injuries after a car accident. Many people in Kansas City walk away from a collision thinking they are fine, only to develop headaches, dizziness, blurred vision, cognitive fog, mood changes, or neck pain within hours or days. These are often signs of a concussion or mild traumatic brain injury. Without early medical care and a structured rehabilitation plan, symptoms can linger for months and sometimes years.
At Keystone Medical Group, we focus on evidence based multidisciplinary TBI rehabilitation that evaluates the entire person, not just a single symptom. Our goal is to help patients restore cognitive function, improve physical performance, reduce pain, and regain independence after a collision. Because we see personal injury patients every day in Kansas City, Overland Park, Lee’s Summit, Independence, and North Kansas City, we understand what people need to recover safely and return to normal life.
This article explains why early TBI rehabilitation matters, what happens when care is delayed, how a multidisciplinary approach works, and why structured treatment is essential for the best outcomes after a car accident.
The Hidden Problem With Delayed Concussion Diagnosis
A concussion rarely shows up on CT scans or standard imaging. Even when a collision seems minor, the brain can experience rapid acceleration and deceleration forces that affect neural pathways. Many patients feel confused, emotional, nauseated, or mentally foggy after the crash but assume the symptoms will fade. In some cases they do, but for many patients the symptoms persist or grow worse.
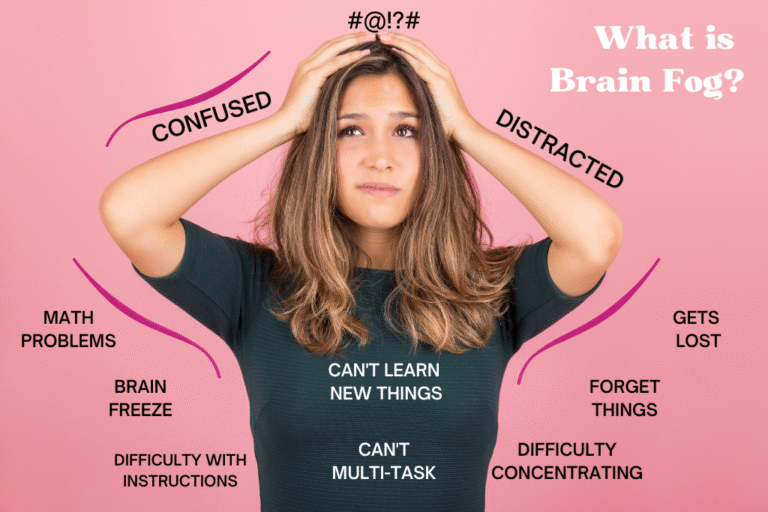
Delayed diagnosis is common because symptoms can onset slowly. Cognitive fatigue, irritability, difficulty concentrating, and sleep changes often become noticeable several days later. When patients wait weeks or months before seeking care, their nervous system can develop compensations that make recovery more difficult. Early intervention interrupts that process.
In Kansas City, many personal injury patients seek care first for neck pain or headaches, only to discover that their discomfort is part of a larger picture involving vestibular, cervical, cognitive, and autonomic dysfunction. Early rehab identifies these overlapping components before they progress.
Why Early Rehab Makes the Greatest Impact
Traumatic brain injury recovery happens through neuroplasticity, which is the brain’s ability to reorganize and create new connections. The sooner the rehabilitation process begins, the more effectively the brain adapts. Early rehab takes advantage of this window of opportunity.
Here are the main reasons starting rehab early after a car accident leads to better outcomes:
The Brain Learns Better in the Early Phase
Within the first days and weeks after injury, the brain is in a heightened plasticity state. Proper stimulation during this period can speed up healing. This is why vestibular therapy, visual rehab, cognitive training, balance exercises, and targeted physical therapy are part of early intervention at Keystone Medical Group.
Early Rehab Prevents Compensations
When patients wait too long, their body and brain develop workarounds. For example, a patient with dizziness may avoid turning their head. A patient with convergence difficulty may reduce reading or screen time. Someone with cognitive fatigue may withdraw from work responsibilities. These compensations introduce secondary problems that prolong symptoms. Early rehab stops these patterns from developing.
Early Rehab Reduces the Risk of Persistent Post-Concussion Syndrome
Many people recover from a concussion within a few weeks. Those who do not often fall into persistent post concussion syndrome, where symptoms last longer than 3 months. Early structured treatment reduces this risk significantly.
The Sooner You Start, the Faster You Get Back to Work and Daily Life
Patients who begin their rehab plan early often regain endurance, concentration, and emotional stability all while experiencing faster reduction in headaches, dizziness, and sleep problems.
What Happens When Concussion Rehab Is Delayed
Delayed intervention can lead to long term consequences. We see this frequently in Kansas City after auto accidents because many people avoid seeking care until the symptoms become overwhelming.
Here are the most common outcomes of delayed rehab:
Persistent Symptoms That Could Have Resolved Sooner
Untreated vestibular dysfunction, oculomotor issues, and neck injuries contribute to ongoing headaches, vertigo, and cognitive fog. These are highly treatable when addressed early.
Increased Sensitivity to Light, Noise, and Motion
The brain becomes more reactive when the sensory systems remain unaddressed. Delayed care makes treatment more complex.
Emotional and Behavioral Changes
Anxiety, irritability, depression, and emotional lability become more difficult to manage when the injury has been present for months.
Sleep Disturbances
Poor sleep slows down all other healing processes. Delayed care often means patients have been dealing with disrupted sleep patterns for far too long.
Difficulty Returning to Work
Patients who wait months before receiving structured treatment often struggle with productivity, multitasking, concentration, and tolerance for busy environments. Early rehab helps resolve these issues before they become major obstacles.
Why TBI Requires a Multidisciplinary Team
There is no single treatment that fixes a concussion. TBI affects multiple systems that interact with one another. This is why Keystone Medical Group has built a collaborative model involving medical providers, physical therapists, rehabilitation specialists, and coordinated referrals when needed.
A multidisciplinary approach ensures that each system involved in a concussion is evaluated and treated properly.
The Cervical Spine
Neck injuries are almost always present after a car accident. Whiplash strains the ligaments, muscles, and joints in the neck, which often contribute to headaches, dizziness, and visual symptoms. Physical therapy plays a major role in restoring mobility, improving posture, reducing muscle spasm, and increasing stability in the cervical region. When necessary, collaboration with chiropractic providers focuses on mobility and alignment through controlled, patient centered approaches.
The Vestibular System
This system controls balance, orientation, and head movement. After a TBI, vestibular dysfunction can cause dizziness, nausea, vertigo, disequilibrium, and motion intolerance. Vestibular therapy retrains these pathways through gaze stabilization, habituation exercises, balance work, and motion sensitivity retraining.
The Visual and Oculomotor System
Convergence issues, tracking difficulties, blurred vision, and visual motion sensitivity are extremely common after concussion. Visual rehabilitation includes eye tracking drills, accommodation training, saccadic exercises, and functional tasks that retrain visual processing.
Cognitive Function
Attention, memory, processing speed, and executive function frequently decline after a TBI. Cognitive rehabilitation is essential for helping patients return to work, school, and daily responsibilities. Therapy includes memory strategies, attention training, task sequencing, dual task challenges, and customized cognitive drills.
The Autonomic Nervous System
Dysautonomia often develops after a TBI. Symptoms include rapid heart rate, temperature dysregulation, dizziness, exercise intolerance, and fatigue. Treatment may include graded exertion protocols, functional exercise, and autonomic retraining guided by clinical evaluation.
By integrating these systems, patients receive a clear path toward recovery instead of fragmented care.
What Early Rehab Looks Like at Keystone Medical Group
Every patient receives a customized rehabilitation plan. While no two plans are identical, the following steps represent the framework we use for early intervention after a car accident.
Step 1: Comprehensive Medical Evaluation
The first visit includes full history, neurological screening, cervical spine assessment, symptom evaluation, and functional testing. When necessary, imaging such as MRI or MRI with DTI may be ordered to assess deeper structural or functional changes.
Step 2: Identification of All Impaired Systems
Instead of focusing on one symptom, we evaluate every system affected by TBI. This includes vestibular testing, oculomotor screening, balance and gait evaluation, cervical assessment, autonomic screening, and cognitive function testing.
Step 3: Immediate Symptom Stabilization
The early phase involves reducing symptoms through targeted interventions that support the patient’s nervous system without triggering setbacks.
Step 4: Introduction of Targeted Rehabilitation
Once symptoms are stabilized, patients begin structured rehab sessions that address the specific systems involved. These may include vestibular therapy, visual rehab, physical therapy, cognitive training, balance work, and graded exertion.
Step 5: Ongoing Reassessment and Progression
Recovery is not linear. Regular follow up allows our providers to adjust plans based on the patient’s progress, work demands, and functional goals.
Step 6: Return to Life and Work Planning
Patients who live or work in busy environments like downtown Kansas City, Overland Park, or Lee’s Summit often experience symptom flare ups when returning to real world settings. We help patients reintegrate gradually by building tolerance and resilience.
How Early Rehab Helps Personal Injury Cases
Proper documentation matters in personal injury. Early rehab creates a clear record of injury, medical necessity, functional limitations, and response to treatment. This helps patients demonstrate the extent of their injuries when working with attorneys or insurance providers.
Here are the main advantages:
• Clear documentation of symptoms
• Identification of all impairments caused by the crash
• Ongoing functional assessments
• Justification for ongoing care, referrals, imaging, and rehabilitation
• A structured timeline that shows the patient followed medical advice
A delayed start creates gaps in the medical record that insurance companies often use to dispute claims.
When to Seek TBI Rehab After a Car Accident
Patients should seek evaluation immediately if they experience any of the following after a collision:
• Headache
• Dizziness or vertigo
• Confusion
• Difficulty concentrating
• Blurred or double vision
• Nausea or vomiting
• Fatigue
• Memory difficulty
• Emotional changes
• Sleep disruption
• Sensitivity to light or noise
• Neck pain
Even mild symptoms can indicate deeper dysfunction. The earlier the patient is evaluated, the more complete and predictable the recovery tends to be.
Why Kansas City Residents Choose Keystone Medical Group
Keystone Medical Group provides a full spectrum of TBI and personal injury rehabilitation for patients in Kansas City, Overland Park, Independence, North Kansas City, Lee’s Summit, Gladstone, and surrounding areas. Patients choose us because we offer coordinated care, faster access to evaluation, and detailed documentation that supports both medical recovery and personal injury claims.
Our goal is simple. Restore function. Improve quality of life. Help patients return to work and daily activities safely and efficiently.
Final Thoughts
Early rehabilitation after a traumatic brain injury is one of the most important factors influencing recovery. A car accident may feel overwhelming, but the right team can guide patients through every phase with clarity and confidence. The sooner the evaluation and treatment begin, the more predictable and complete the outcome becomes. Keystone Medical Group is here to support patients throughout the Kansas City region with evidence based, multidisciplinary care designed specifically for TBI and personal injury cases.
Disclaimer: This blog is for educational purposes only. It is not medical advice and should not be used to diagnose or treat any condition. Every patient and every injury is different. If you have symptoms after a car accident or traumatic brain injury, schedule an evaluation with a qualified medical provider. If this post discusses supplements, medications, exercises, or therapies, consult your doctor before starting anything new. Reading this blog or contacting our clinic does not create a patient provider relationship.